Concussed: Collective Competence in Healthcare
and the Patient Experience
Jessica B. Schwartz PT, DPT, CSCS
On May 16, 2015, I had the privilege to speak in front of 200 of my colleagues at Evidence in Motion’s 3 day hands-on and didactic learning festival, Manipalooza, at the University of Colorado’s Anshutz Medical Campus in Denver, Colorado.
If I had to sum the entire weekend up in one word it would be:
Inspired.
Topics of discussion and practical application included concussion, neuroscience, biases in healthcare, manipulation, pelvic health, workplace safety, advanced soft-tissue mobilization, and an epidemiological review of low back pain: where it’s been, where we are going, and how the physical therapist is leading the way.
I was inspired by the impressive cohort of speakers (Timothy Flynn, John Childs, Larry Benz, Adrian Louw, Jennifer Stone, John Groves, Julie Whitman, Teresa Shuemann, Tim Fearon, and humbly- myself) and that of the volunteer Fellows, past and present, to assist with knowledge dissemination and translation throughout the entire weekend.
I have learned that when you are surrounded by some of the top minds in the world who collectively come together with two interests in mind: 1. How to immediately make the clinician better for next day patient care and 2: the importance of being connected to oneself, as provider, including self-awareness of biases and our past patient/life experiences which in turn correlate to increased self-management increasing efficacy in and out of the clinic…it’s well, inspiring.
This low-ego, incredibly fun, and contagiously charismatic group of doctors, clinicians, and scientists was truly an impressive group to be a part of in all domains to engage with, learn from, and disseminate knowledge to a hungry audience of motivated professionals.
May 16, 2015 was particularly profound for me because I essentially got to go public with my story for the first time…and who better to present to than “my own people”, Physical Therapists.
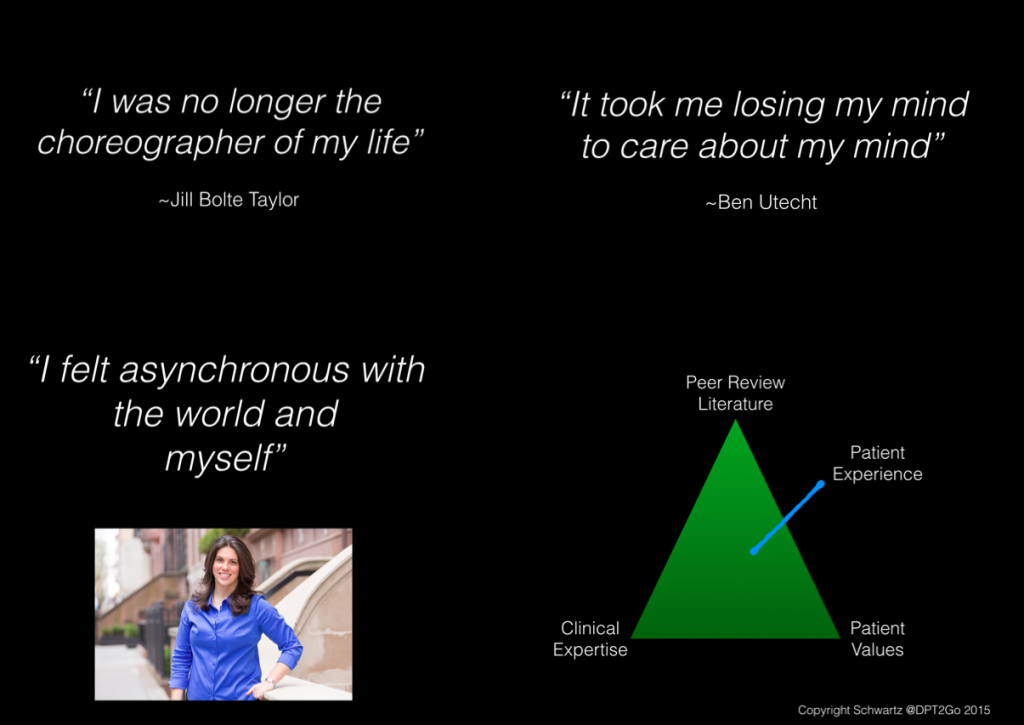
The Schwartz adaptation of the David Sackett’s, MD Evidence Based Medicine (EBM) triangle including patient experience. I encourage all clinicians to listen to and learn from our patients stories. We can learn so much by deeply listening to our patients as people first.
I was in a motor vehicle accident October 3, 2013 and my life changed forever. I underwent a year of rehabilitation living with post-concussive syndrome. I had the good fortune to be cared for by the incredible team of physicians, non-physician doctors, and clinicians at the New York University Concussion Center for 10+ hours a week for about a year of rehabilitation and guidance so I could successfully Return to Life with my new abilities.
I said it time and time again during my physical, orthopedic, neurologic, and cognitive rehabilitation throughout the year… “if I don’t share this story with the medical community it’s essentially malpractice in my eyes”. I continue to hold strong to these goals and values of transparency, story-telling, and sharing of my own personal journey with the goal of increasing concussion patient-provider connectedness in the medical community.
I have one goal: facilitate collective competence amongst the healthcare community in order to better identify, treat, and manage the concussion patient along the entire continuum of recovery from acute to chronic.
I was able to update the audience on some of the latest happenings in concussion research and development, review some stigmas associated with post-concussive syndrome, present my case revealing the patient was myself about half way through the presentation, share some poignant moments of what it was like to live through post-concussive syndrome, and announce the Evidence in Motion Concussion Certificate Program for the post-professional medical provider.
I am absolutely thrilled to be leading this program with the key concept of instilling collective competence across the healthcare continuum so we as clinicians can 1. better understand the scope of everyones interdisciplinary practice, 2. increase abilities to identify commonly missed post-concussive symptoms (cognition, vision, vestibulo-ocular, persistent pain, etc), 3. empower the provider to feel confident in his/her abilities when evaluating, treating, and appropriately referring the concussion patient to a colleague as needed, and 4. empower the provider to educate the community from sports leagues, coaches, parents, school districts, fellow medical professionals, care-takers, employers, and patients.
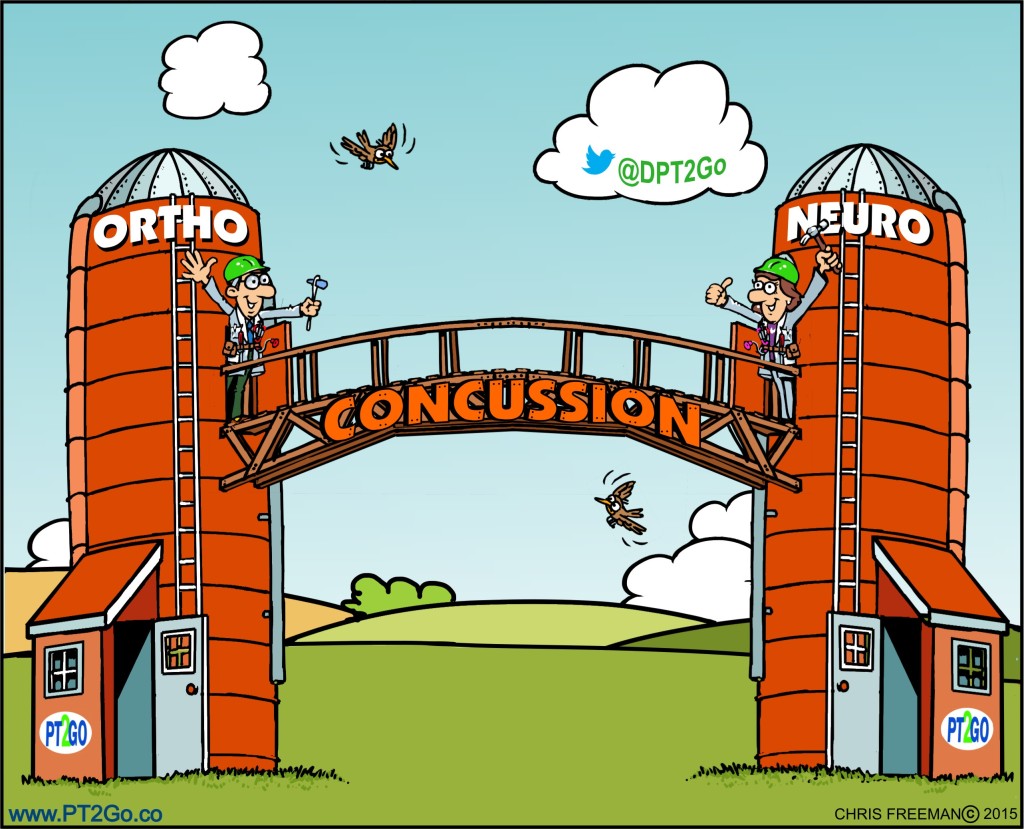
A key theme of my professional being and future lecture series as it pertains to the concussion patient is built around the concept that there is no one provider who can comprehensively treat this population of patient. My core clinical values foster interdisciplinary knowledge translation. How can we refer to one another if we sincerely don’t have a grasp of what each of us across the healthcare continuum can do for one another as provider and for our mutual patient? I would like to facilitate this forward and collective thinking necessary to provide the concussion patient the best possible care.
Faculty will include some of the top minds, researchers, and clinicians in the world collectively coming together to educate the post-professional academic learner. Faculty will include the neurologist (adult and pediatric), emergency medicine physician, vestibular physical therapist, traumatic head and neck disorder scientists, occupational therapist/vision therapy, neurogenic speech language pathologist, board certified sports clinical specialist physical therapist, certified athletic trainer, neuroscientist, and the neuropsychologist.
Specialty topic areas will include: Pediatrics, Geriatrics, Sports, Trauma, and the Service Member/Veteran.
Collectively, these incredibly bright and motivated minds will come together and I, as program director, will bridge the gaps empowering the clinician along the course of one year to become comfortable with their clinical abilities, their interdisciplinary colleagues, and most importantly- this cohort of concussion patient who is so often mismanaged in this maze of disconnected care episodes that healthcare system of today has unfortunately bred.
Future information will be launched soon on the Evidence in Motion’s website for a Summer 2015 launch date.
I look forward to being a part of an incredible movement to educate the healthcare practitioner in an online and in-person synchronous and asynchronous learning environment.
Cheers to a tremendous year to come for both the patient and provider with respect to the identification, treatment, and management of the concussion patient!
Thank you for time, attention, and coming along this exciting journey of advocacy as post-concussive survivor, story-teller, and educator.
*Please excuse the cough. The Colorado altitude got the best of me
Kind Regards,
Jessica B. Schwartz PT, DPT, CSCS
*Special thank you’s to Tim and John for the invite to Colorado!