Original artwork by Jessica Schwartz Rendered by Chris Freeman
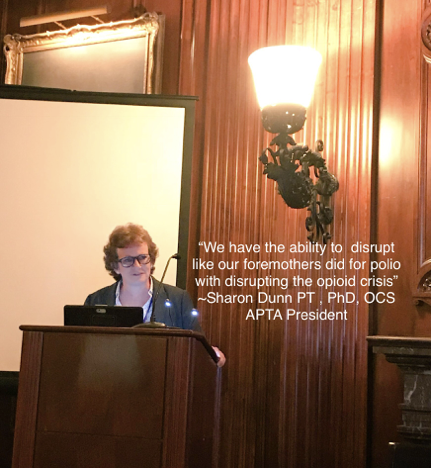
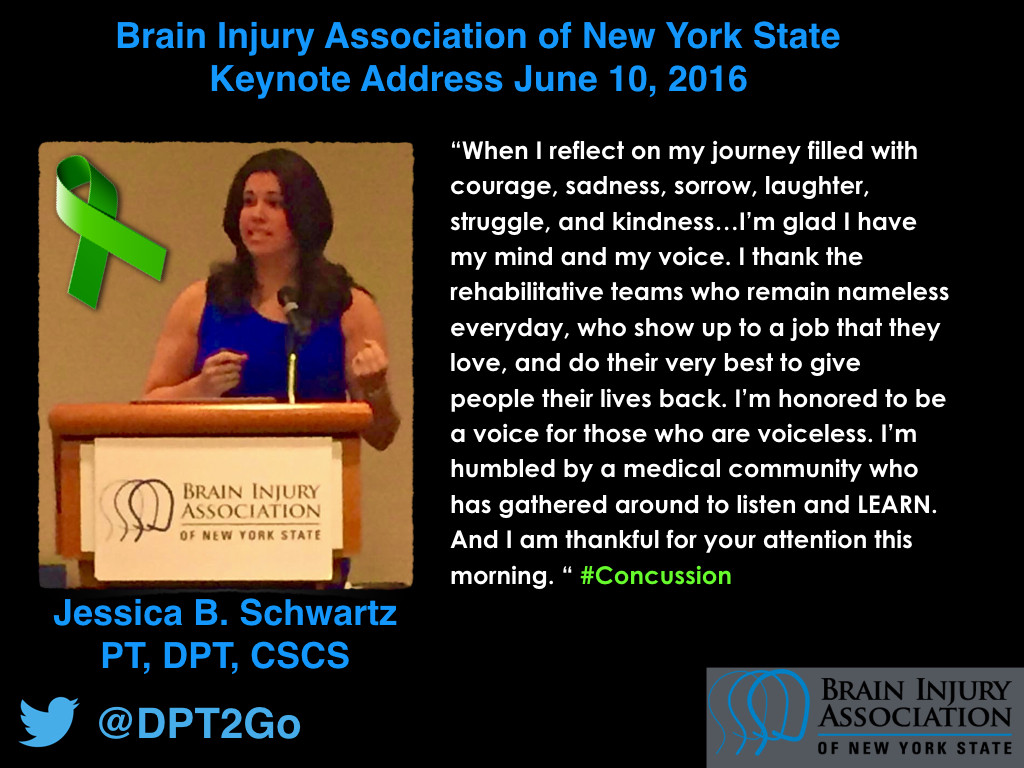
Jessica B. Schwartz PT, DPT, CSCS
There is a paucity of quality concussion education in entry level, residency, and post-professional medical education.
Why?
Because there is no evidence based medicine for concussion.
A bold statement as I introduce what I believe to be the worlds first yearlong, multidisciplinary, and post-professional concussion education program for clinicians.
Let me start with a story:
It was the week I got promoted to junior partner of my company.
The week I took a deep breath for the first time in my life and said “OK Schwartz…You’ve arrived.”
I was surrounded by people whom I genuinely cared about, professionally and personally, and I felt like my nose to the grindstone personality the last 13 years of formal didactic education, business mentorship, and the chase to this finish line had come to fruition.
That was the week I was hit by a car.
That was the week my life changed forever.
On October 3, 2013, I went from being Dr. Schwartz to patient 237427 in a NYC Emergency Department getting rolled through a CT Scan.
It’s a difficult journey being on “the other side of healthcare.”
I was that patient rolling to CT with my MD Calculator in hand who was able to recite the Canadian CT Head Rules like a proud elementary school student who had just learned her speaking part for the school play.
Physical therapy was my craft. I was mastering the craft of treating the patient as person, developing my patient rapport tools, building a wonderful international referral network, and understanding the nuances of running multiple successful businesses.
I loved every minute of it. The more I learned the more I wanted to learn.
A one week medical leave of absence turned into 10+ hours of rehabilitation a week for a year.
How could an injury so seemingly benign change my life forever?
What We Know:
In 1997, the CDC reported 300,000 concussions in the United States. In 2016, the CDC estimates are 1.6-3.8 million sports related concussions based off of the most recent 2006-2010 data.
I strongly believe that these numbers continue to be greatly underestimated based off of the heterogenous nature of this injury, underreporting[1-4], ~25% of people not seeking emergency department or other medical care[5], and lack of an agreed upon definition and consensus on what the injury is in the literature[6-8].
We know that approximately 20-30% of patients develop persistent symptoms crossing over into the post concussion syndrome threshold each year with ranges from 5-58% in the literature[9-11].
If we look at ~30% of all concussions crossing over into the persistent symptom category, that is 1.14 million people in the United States based off of the current data alone.
Remember, I continue to believe that this data continues to be grossly underestimated.
The Gaps:
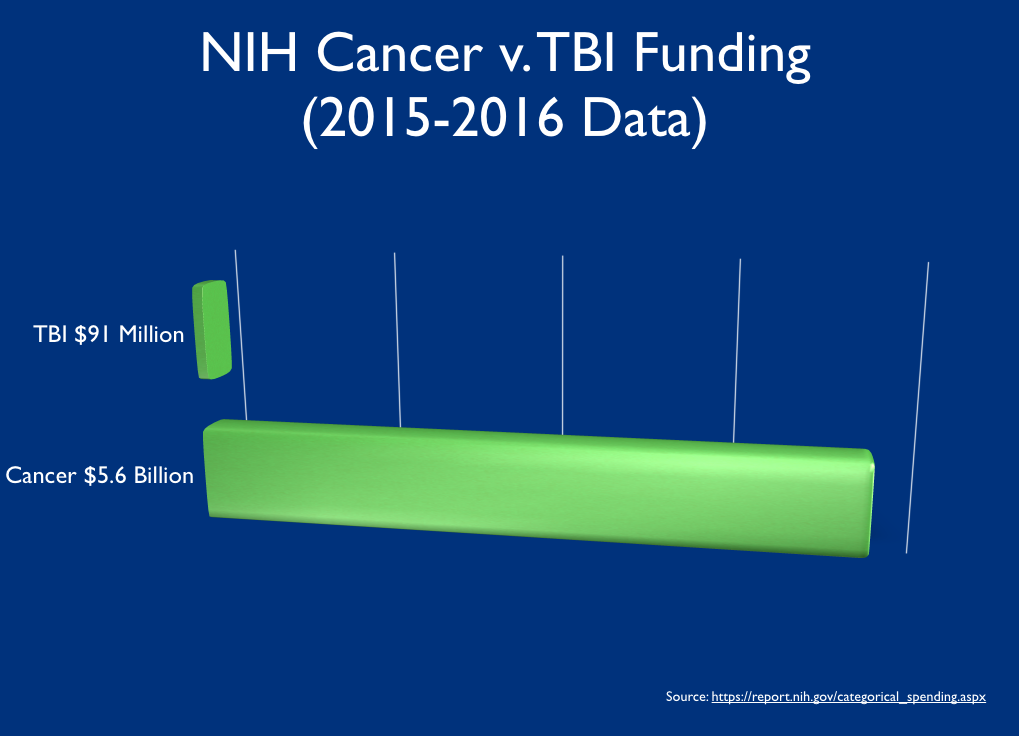
We know that TBI is grossly underfunded yet it is a major cause of death and disability in the United States, contributing to about 30% of all injury deaths[12].
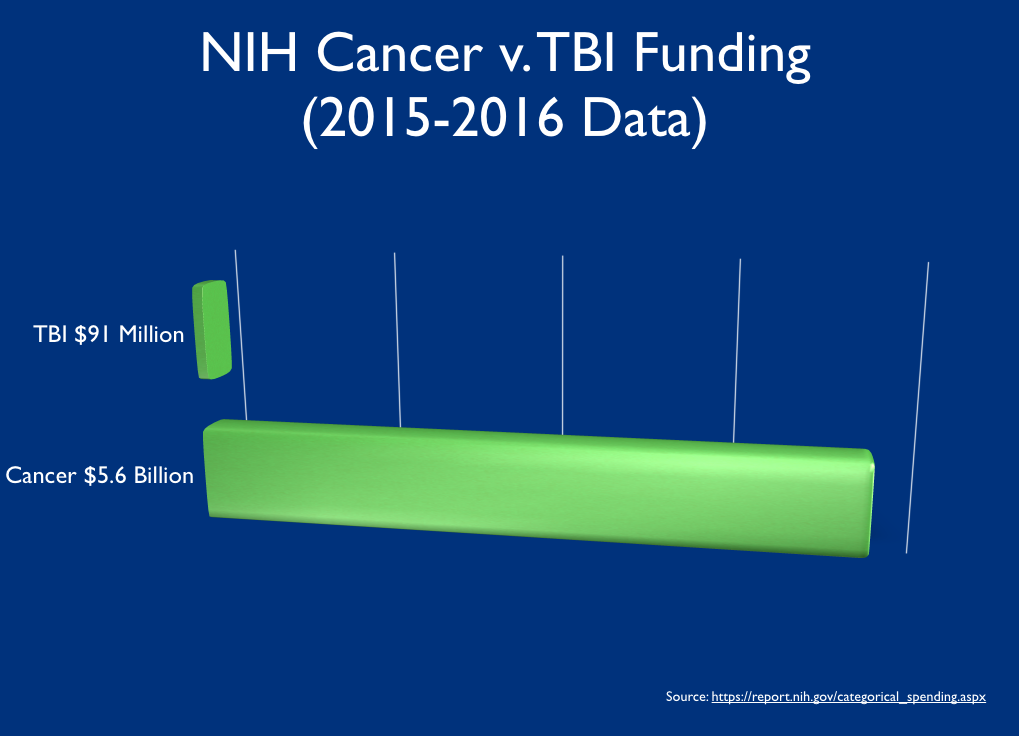
According to the National Institutes of Health (NIH), Cancer research received $5.6 Billion in 2015. Comparatively and up from $88 million in 2015, TBI is estimated to receive just $91 million in 2016[13]. Approximately 5.6 million people are living with the long terms effects of TBI and 138 deaths occur per day[12] amounting to ~50,000 deaths per year in the US. In 2015, there were 1,658,370 new cancer cases diagnosed and 589,430 cancer deaths in the US[14].
Why compare cancer and TBI? Because cancer has made huge gains by breaking down cancer. We don’t treat cancer. We treat large cell non-Hodgkin lymphoma. We need to do the same in the concussion community.
Scientifically, we must start with agreeing upon a universal definition of concussion, mTBI, and TBI. From there we need to be able to break down the injury appropriately based off of neurophysiological changes and injury to specific areas of the brain. While these are lofty goals, I also don’t see this being tangible in the near future nor is it clinically and functionally relevant to the patient seeking care in front of us today.
The above statistics indicate that we are doing much better at saving patients lives from severe cases of TBI vs cancer; however, the true burden exists with TBI survivors suffering from the lasting effects of what a TBI does to a person as a whole being.
We know that 100% of all neuroprotection phase III studies are negative, less than 5% of New Medical Entities (NME) in clinical assessment make it to FDA approval, and 100% of all Phase III trials in TBI are negative.
This means that there have been zero phase three clinical trials in TBI that have moved on to completion, there are zero drugs for TBI, and that TBI and concussion are strictly a clinical diagnosis.
We have to do better. And we can.
Medical Education and Healthcare:
Daniel Goleman discusses the key concept of “iatrogenic suffering” in medicine. This is an added anguish by medical personnel delivering insensitive messages that can often engender more emotional suffering than the actual illness itself[15].
Historically in medicine if we do not understand an injury or disease pathway, we prescribe rest or send the patient to a psychologist e.g. syphillis, low back pain, B12 deficiency, cardiac issues in women, etc.
We’ve missed the mark in the concussion community as medical providers. Over the last few decades, we’ve allowed the medico-legal literature to get ahead of us in the medical community.
It wasn’t until 1989, a neuropsychologist by the name of Jeffrey Barth, was part of the first group to suggest that cognitive testing in preseason athletes may have some value due to concussive injuries presenting lasting effects.
We’ve enabled a culture of “I got my bell rung” to prevail and have not addressed concussion from a systems level until recently.
I’ve heard time and time again that “We can’t teach it because there’s no empirical evidence”.
Nonsense.
As I was being well-cared for by my team of physicians and clinicians, I continued to do my best to take a step back and look at the inner workings of the healthcare team, system and educational offerings that are made available to all clinicians from physician to PT et al.
When I learned that 2015 was the first year that neurology residencies were receiving formal didactic education in concussion within the ‘Behavioral Neurology’ section springing from the work and advocacy of the Sports Neurology Section of the American Academy of Neurology, I knew there had to be something done.
A change.
A change in the global architecture of medicine with respect to the concussion patient of today.
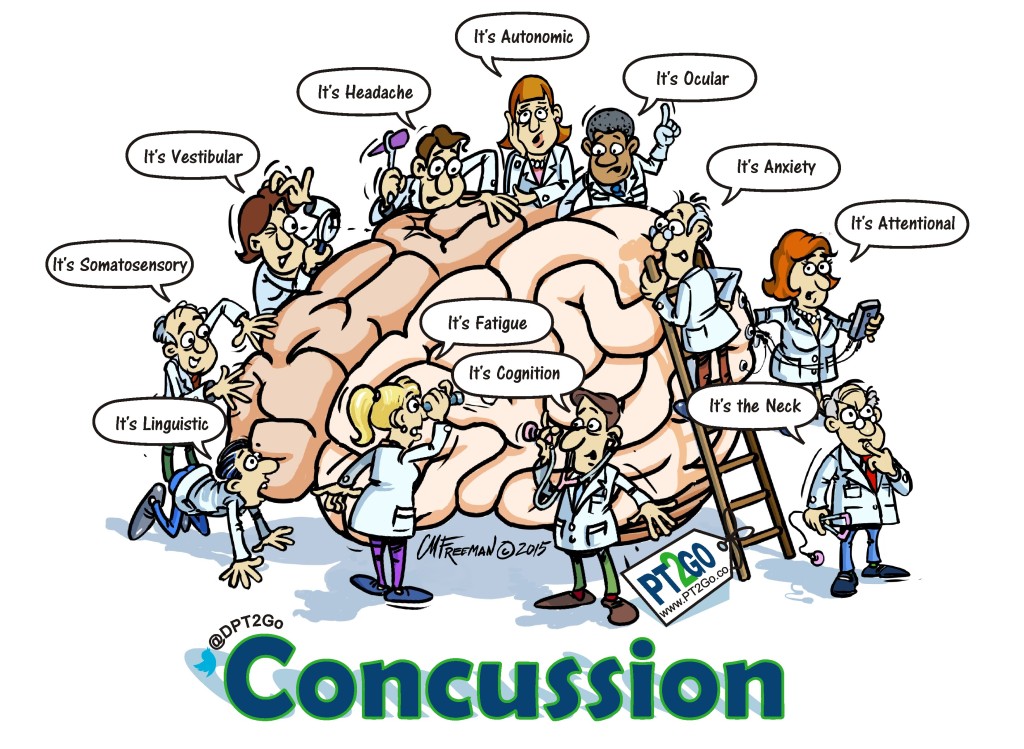
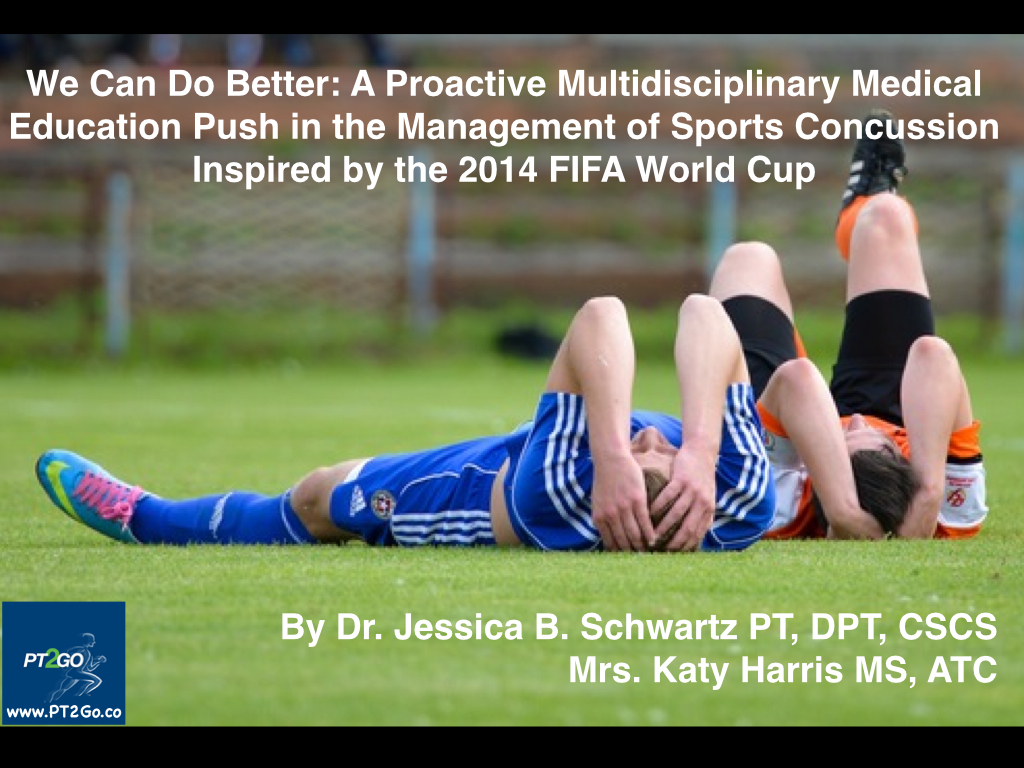
A concussive injury is an all hands on deck injury. It can often require a team of clinicians to identify, treat, and manage this patient population.

Concussion patients port of access to the clinician of today is infinite. It can range from the athletic trainer, the emergency department physician, the primary care physician, the pediatrician, the nurse practitioner, the physician assistant, the school nurse, psychologist, physical therapist, occupational therapist, speech therapist, and anyone who has direct access to the patient of today.
I emphatically deliver this message when I speak publicly: it is not a matter of if you treat concussion patients. It is a matter of when you will encounter, treat, and/or refer a concussion patient.
A concussion is not a broken bone. That’s easy. We know normal tissue healing parameters in healthy populations.
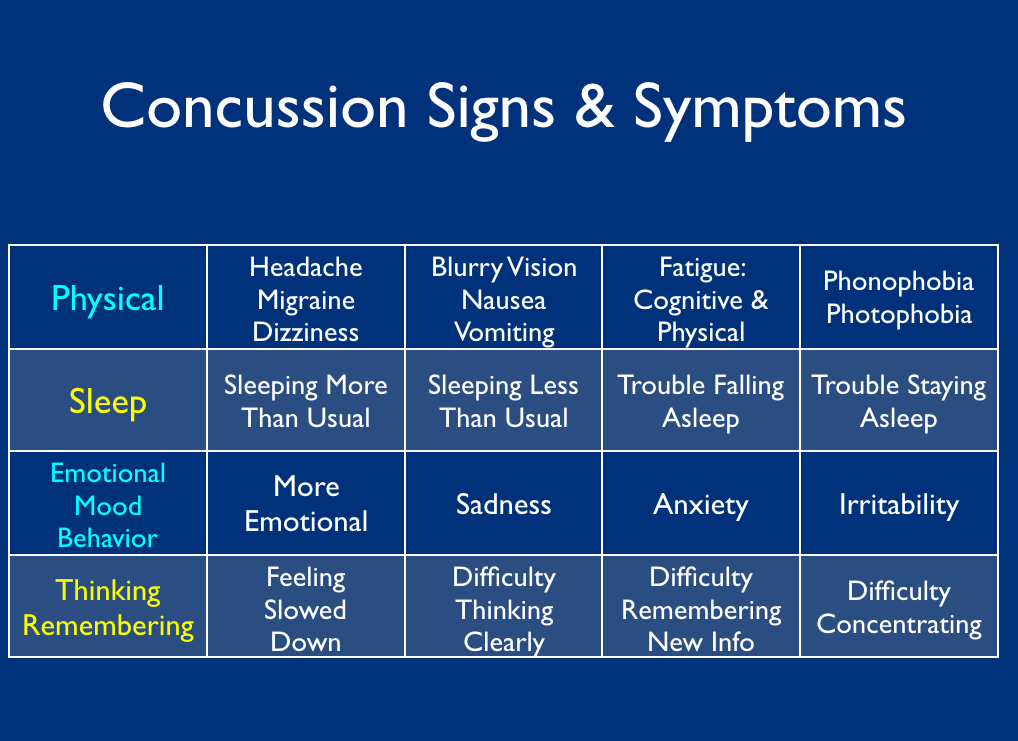
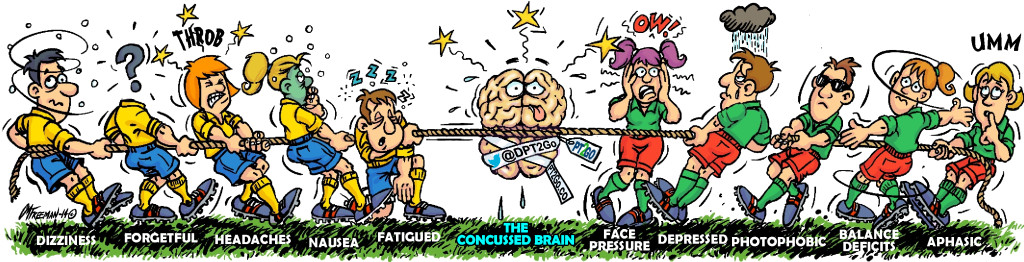
A concussion is a neurophysiologic injury that can affect all domains of a person’s life from somatic, cognitive, emotional, vestibular, sleep, and behavior often with non-specific answers to the all important patient question of “when will I get better?”
It is gut-wrenching as a clinician to have the self awareness to look into a patient’s eyes and say “I don’t know.” It is even more painful as a patient to be completely unaware of if you will ever get better when you are being cared for by one of the best clinicians in the world.
We can do better. And we will. Here’s how.
Healthcare Teams:
Long gone are the days of the one physician model, yet we seem to be in a conundrum when it comes to communication and teamwork in medicine.

The Doctor Sir Luke Fildes (1891) https://commons.wikimedia.org/wiki/File:The_Doctor_Luke_Fildes_crop.jpg
In the fall of 2014, I had the privilege to virtually attend the International College of Residency Education’s (ICRE) opening plenary delivered by rhetorician scientist Dr. Lorelei Lingard on Collective Competence: Adapting our concept of competence to healthcare teams[16].
During this time, I was finalizing my concussion rehabilitation and Dr. Lingard’s words helped facilitate my eureka moment of how I can aide in providing a solution to this medical world of specialists all attempting to treat the same poorly defined and heterogenous injury.
Summatively, she states that individual competence does not equal good healthcare.
She elaborates reviewing a case scenario describing the maze of disconnected care episodes that the patient of today is experiencing.
Dr. Lingard states that we need to “evaluate in situ, broaden focus beyond individual actions to include inter-actions among individuals, capture the ‘cracks’ between the care episodes, and consider interactions among elements of the system, not just among people…Competence is a way of ‘seeing’ that both directs and deflects our attention. The cracks between care episodes, experts cultivating collective competence ‘know how the system usually fails in this situation, and plans accordingly.’ Our attention is directed towards individual competence and deflected from collective competence. We need both[16].”
My role is to facilitate collective competence in the concussion community.
Let’s think about the concussion patient of today.
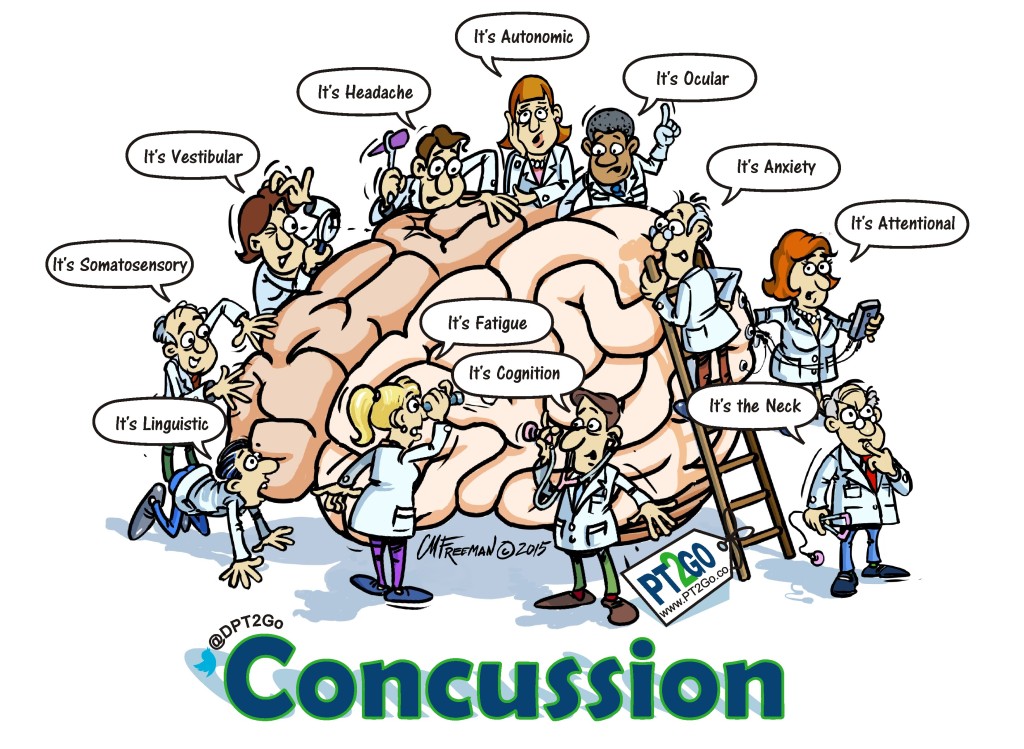
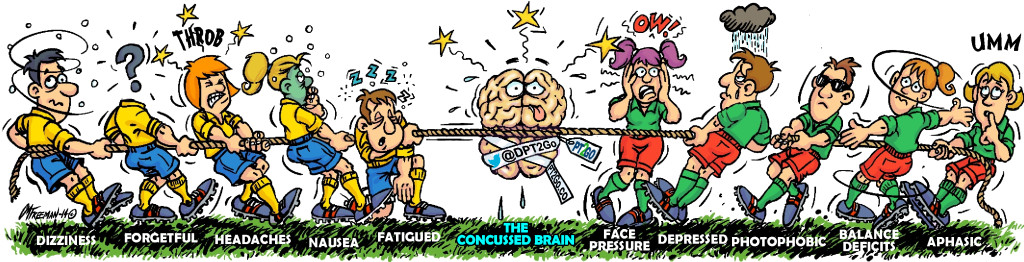
A concussed individual can experience any one of the following myriad of symptoms all at once or over a period of time [See Chart].
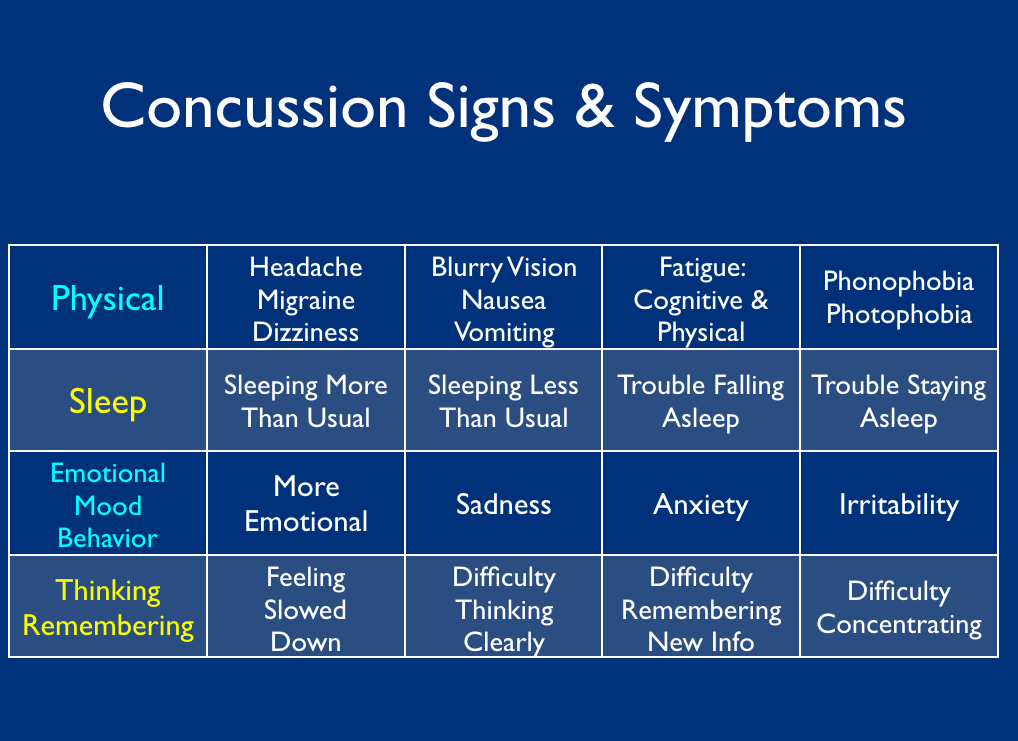
Each of these symptoms can be managed by individual specialists that may or may not cohesively integrate their treatment models with a co-treating clinician.
Concussion identification, treatment, management, and having the self awareness to know when and whom to refer appropriately can be a complex team model and clinical algorithm.
Each concussion case is unique and treatment models are 100% situationally dependent.
Kenneth Burke, an American literary theorist, once said that “every way of seeing is a way of not seeing.”
We can’t simply “treat the headache” or “treat the balance issue.” Treating the concussion patient of today involves a complex series of evaluations across all domains in order to systematically identify injury deficits in order to appropriately make the decision of what to treat, when to treat it, and when to refer appropriately.
If you treat together, you must learn together.
Here’s how.
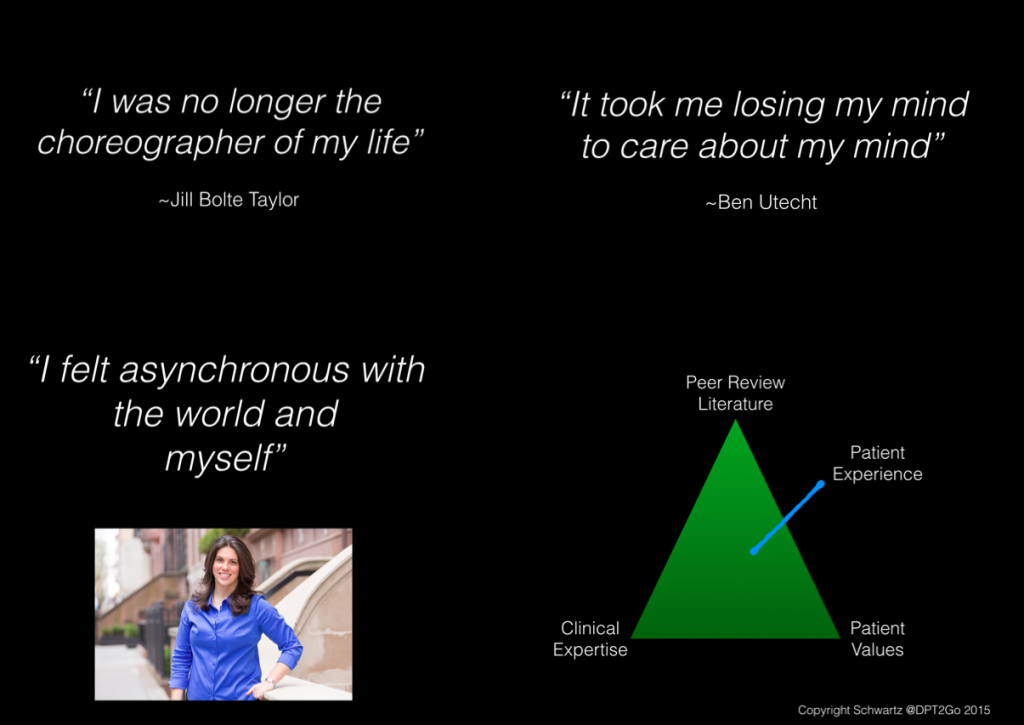
Rapport and Clinician Synchronicity:
“To feel with, stirs us to act for[15].”
Get in-synch with your concussion patients.
These patients often feel very disconnected to the medical community. Patient stories of seeking care from 5+ medical providers until they “find their person” in healthcare is not uncommon.
Rapport is key to successful patient, provider and caregiver interactions. When people are in rapport, their physiology actually attunes. Robert Rosenthal published a landmark article revealing the central tenets of “relationship magic,” the recipe for rapport. This only exists when three elements are present: mutual attention, shared positive feeling, and a well-coordinated nonverbal duet. As these three emerge cohesively, we spark rapport[15].
This is how lifelong patient-provider and provider-provider relationships are formed.
Nature is based upon energy and timing. Basic science has identified symbiosis throughout the natural world ranging from the firing of an action potential to the marvelous making of what happens between winter and spring.
Concussion is an injury of asynchronous firings at a cellular level which accumulate amounting to a functional dysfunction with ones self and environment.
Original Concept by Jessica Schwartz; Rendered by Chris Freeman
We need to learn how to adapt to the needs of our patients who carry a host of pre and post morbid medical conditions and circumstances presenting with the complexities that the heterogenous nature of a concussive injury presents.
The Program:
The Evidence In Motion Concussion Certificate Program is committed to educating the post-professional multidisciplinary clinician of today in concussion identification, treatment, and management by fostering a rehabilitative team approach.
This 12-month program provides the latest clinical conversations, evidence-based guidelines, and consensus statements while integrating real world experiences from patients, providers, and caregivers who have navigated the complex healthcare network of today.
Content delivery is both interactive and dynamic, exposing the student to some of the most influential clinicians in the concussion community coupled with the unique learning experience of provider to provider, patient to provider, and caregiver to provider storytelling.
By fostering a rehabilitative team approach, the EIM Concussion Certification hopes to facilitate collective competence across the healthcare continuum in order to better triage, treat, and appropriately refer the concussion patient of any age from acute to chronic stages.
This year long multidisciplinary concussion certificate sets the learner up for success utilizing an asynchronous and synchronous online learning environment for the busy post professional of today.
The in-person weekend intensive reviews the psychomotor properties of the concussion evaluation, treatment, management, and referral options based off of the providers scope of practice during the 12 month didactic education experience.
As a pre-requisite to the program, each post-professional student will undergo a therapeutic neuroscience education course. As we embark on a multidisciplinary educational journey together, I sincerely believe that we all speak the same language of medicine; however, we bring many different dialects to the clinical table.
Current best-evidence shows that therapeutic neuroscience education improves pain ratings, function, pain catastrophization, physical movement and cost of healthcare utilization.
I will utilize the TNE course to cohesively meld the post-professional multidisciplinary EIM Concussion students in language, compassion, and competency of the therapeutic neuroscience evaluation in order to jumpstart their experience of learning together in a new environment.
A few months before physician Kenneth Schwartz died, he stated that “Quiet acts of humanity have felt more healing than the high dose of radiation and chemotherapy that hold the hope of a cure. While I do not believe that hope and comfort alone can overcome cancer, it certainly made a huge difference to me[15].”
I hope to create kind, compassionate, and clinically efficient clinicians who foster rapport with patients, interdisciplinary colleagues, and across disciplines.
Care for the concussion patient. Care for him/her together. And care for him/her well.
The Faculty:
I’ve been fortunate enough to have returned back to patient care and have surrounded myself with some of the brightest and most dedicated faculty in the world in their respected specialties.
Over the last year, the energy that I’ve felt from this group of men and women has been palpable. I am honored everyday to have worked with and continue to collaborate with each and everyone of these passionate clinicians.
What do they all have in common? I systematically screened all interviewees for passion, high IQ, high EQ, and low ego who have the self awareness to take a step back from themselves and look at the big picture of clinical care.
We have a tall order in front of us and I know we’re here to do our best to help clinicians of today put our best foot forward to educate each other and our communities of coaches, parents, spouses, teachers, caregivers, and loved ones on the multifaceted injury that concussion can present itself as to the provider and patient of today.
Why Story?:
Paul Zak, a neuroeconomist, eloquently stated “Stories are powerful because they transport us into other people’s worlds but, in doing that, they change the way our brains work and potentially change our brain chemistry — and that’s what it means to be a social creature[17].”
Storytelling allows us to step back, view, and listen from an aerial and reflective standpoint while creating the neural groundwork of patient exposure by connecting to the story, the provider, the caregiver, and the patient.
Schwartz Rounds were invented by an ill physician who also experienced the dichotomy of both doctor and patient. His purpose was to facilitate understanding of how the patient perceives their own illness and treatment by deploying empathy and building rapport[15].
If we have no empirical data, then we need to learn from each other. I believe by deeply listening to each other, patients, and caregivers fosters an excellent way to change the way in which we begin to shift the global architecture of medicine with respect to the concussion patient of today.
How can we help and treat a mutual patient if we don’t sincerely understand what each of us can collectively do for one another in the best interest of the patient.
Story allows us to experience the injury through the eyes of experienced providers, patients, and caregivers who have navigated the complex healthcare system of today.
We need to learn from each other.
When we learn together we can treat together.
Welcome to the beginning of the Evidence in Motion Concussion Certificate Program.
“I did then what I knew how to do. Now that I know better, I do better.” ~Maya Angelou
#Concussion.
Bibliography
1. Register-Mihalik, J.K., et al., Using theory to understand high school aged athletes’ intentions to report sport-related concussion: implications for concussion education initiatives. Brain Inj, 2013. 27(7-8): p. 878-86.
2. Llewellyn, T., et al., Concussion Reporting Rates at the Conclusion of an Intercollegiate Athletic Career. Clin J Sport Med, 2014. 24: p. 76-79.
3. Kroshus, E., et al., Concussion reporting intention: a valuable metric for predicting reporting behavior and evaluating concussion education. Clin J Sport Med, 2015. 25(3): p. 243-7.
4. Kroshus, E., et al., Norms, athletic identity, and concussion symptom under-reporting among male collegiate ice hockey players: a prospective cohort study. Ann Behav Med, 2015. 49(1): p. 95-103.
5. Sosin, D.M., J.E. Sniezek, and D.J. Thurman, Incidence of mild and moderate brain injury in the United States, 1991. Brain Inj, 1996. 10(1): p. 47-54.
6. Menon, D.K., et al., Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil, 2010. 91(11): p. 1637-40.
7. Quarrie, K.L. and I.R. Murphy, Towards an operational definition of sports concussion: identifying a limitation in the 2012 Zurich consensus statement and suggesting solutions. Br J Sports Med, 2014. 48(22): p. 1589-91.
8. Rose, S.C., A.N. Fischer, and G.L. Heyer, How long is too long? The lack of consensus regarding the post-concussion syndrome diagnosis. Brain Inj, 2015: p. 1-6.
9. JJ, B., et al., Epidemiology and predictors of post-concussive syndrome after minor head injury in an emergency population. Brain Inj, 1999. 13(3): p. 173-189.
10. Iverson, G., Outcome from mild traumatic brain injury. Curr Opin Psychiatry, 2005. 18(3): p. 301-317.
11. Babcock, L., et al., Predicting postconcussion syndrome after mild traumatic brain injury in children and adolescents who present to the emergency department. JAMA Pediatr, 2013. 167(2): p. 156-61.
12. CDC. Traumatic Brain Injury in the United States: Fact Sheet. 2016 January 11, 2016].
13. NIH. Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC). 2015 [cited 2016; Available from: https://report.nih.gov/categorical_spending.aspx.
14. ACA. Cancer Facts & Figures 2015. 2016 [cited 2016 January 11, 2016].
15. Goleman, D., Social Intelligence: The New Science of Human Relationships. Kindle ed. 2006: Random House.
16. Lingard, L., Collective Competence: Adapting Our Concept of Competence to Healthcare Teams. 2014.
17. Zak, P. The Neurochemistry of Empathy, Storytelling, and the Dramatic Arc, Animated. 2012 [cited 2016; Available from: https://www.brainpickings.org/2012/10/03/paul-zak-kirby-ferguson-storytelling/.