My Experience at the Inaugural MomsTeam Institute Youth Sports Safety Summit at Harvard Medical School September 15, 2014
By Jessica B. Schwartz PT, DPT, CSCS

Brooke de Lench & Jessica B. Schwartz at The Youth Sports Safety Summit at Harvard Medical School
New York, NY September 19, 2014- As an orthopedic residency trained doctor of physical therapy who is passionate about my career in medicine, injury prevention and knowledge translation in academic medicine, it was a humbling experience to be surrounded by such an enthusiastic, knowledgeable and emotionally intelligent group of people advocating for one common goal: Youth Sports Safety.
Brooke de Lench, the Executive Director of the MomsTeam Institute, and her team launched the inaugural Youth Sports Safety Summit in the Joseph B. Martin Conference Center at Harvard University’s Medical School. The conference perfectly coincided with Ms. De Lench’s directorial debut of The Smartest Team: Making High School Football Safer airing on PBS, Amazon Prime and Vimeo this Fall. The Smart Team program is modeled on the community-centric approach to improving youth sports safety expanding on the Six Pillar approach to all sports injury and concussion risk management.
During the pilot-phase (Fall 2014) MomsTEAM Institute has selected leading researcher coordinators who are working with the following universities to bring the SmartTeams program into their communities: AT Still (AZ), University of Tennessee, University of Texas, Michigan State, University of South Carolina and the University of Tulsa.
In collaboration with and input from all relevant youth sports stakeholders, the Institute has been designing and developing a set of comprehensive health and safety best practices, and will be awarding “Smart Team” status to Youth Sports Organizations (YSOs) which have demonstrated a commitment to minimizing the risk of physical and psychological injury and sexual abuse to young athletes by implementing the best available knowledge and data to provide current best practices.
SmartTeams pilot program is for the Pre-HS athletes (ages 7-14). The Pilot programs will be for select football teams and the national rollout will be with all sports teams (soccer, ice hockey, baseball, lacrosse, etc) in 2015.
During my decade of formal education and subsequent years practicing, I’ve learned that the world of medicine can have similar governmental “bipartisan issues” of not reaching across the aisle to help out a fellow clinician.
The “great ones” across all aspects of medicine seem to have common attributes- professionally and personally. A clinicians ability to listen and be appropriately empathetic while having passion for their field of medicine is rare. Couple this with the desire to learn from others from multiple disciplines and this empirically leads to success for patient outcomes, professional growth, and knowledge translation.
I was both humbled and impressed by Ms. De Lench’s passion and abilities to put together such a comprehensive summit from all walks of life ranging from Harvard physicians, collegiate athletic trainers, an internationally recognized physical therapist, lawyers, neuropsychologists, nutritional experts, motivational speakers, and professional athletes all coming together with the common goal of addressing the youth athlete from an all encompassing holistic approach of mind, body, psychological, emotional and sexual well-being.
I am so very fortunate that I am able to surround myself with inspirational individuals across all aspects of medicine who are innovators in their fields via connections I have made across social media, residency, academia, and alongside my colleagues and associates I am lucky to work with everyday.
It is apparent that Ms. De Lench has similar attributes and has also surrounded herself with a strong group of individuals from all over the country. The central tenet from the inaugural MomsTeam Youth Sports Safety Summit was that it takes a village…or in this case a team of individuals from all walks of life to come together to advocate to the masses from a grassroots level.
If we practice solely in these silos that we set up for ourselves professionally across medicine, law, athletic training, coaching, government policy, and education then we will never be able to reach whole communities in such a positive way in which change needs to occur culturally, fiscally, and individually for the safety of our athletes.
I commend the incredibly comprehensive and still growing team of MomsTeam Institute for advocating and making change for the safety of athletes all across the United States.
Cheers to the continued growth, advocacy and gusto of all the participants who made the inaugural Youth Sports Safety Summit such a positive and educational experience.
Connect with the Youth Sports Safety Summit Speakers and Participants via Twitter:
@MomsTeam @Dr_Capt_Ron @SportingJim @NeeruJayanthi @DPT2Go
@BrookedeLench @JoeEhrmann76 @HollySilversPT @RosalindWiseman
Summative Themes and Highlights in 100 Words or less:
Lyle J. Micheli, MD: Youth Sports Safety: Two Steps Forward, One Step Back
• Discussed the history and evolution of Sports Medicine
• Discussed first epidemiological studies of sports injuries historically touching upon the Princeton v. Rutgers game of 1869 and Harvard v Yale in 1874
• Gracefully walked us along the historic perspectives of sport and injury prevention through the Greek, Renaissance and Modern times
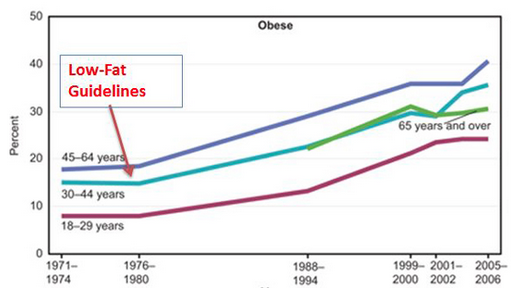
• We have athletically gifted athletes who are not fit and at a high risk for injury
Director of the Division of Sports Medicine at Boston Children’s Hospital; Clinical Professor of Orthopaedic Surgery at Harvard Medical School; O’Donnell Family Professor of Orthopaedic Sports Medicine at Boston Children’s Hospital; Secretary General for the International Federation of Sports Medicine (FIMS)
Jim MacDonald. MD, M.P.H., FAAFP, FACSM: Injury Prevention Strategies For The Pediatric Athlete
• We need to think like Sweden (the safest place to drive on earth). Zero needs to be our north star (regarding injury prevention across a lifetime)
• 98% of kids will not be elite pro athletes. We can’t have our young kids doing sport specialization in their prepubescent years
• ‘If you build it they will NOT come’ is the central tenet in public health: education is not enough
• We need more comprehensive public health initiatives. If we bring together 3 public health strategies (see below), we will see injury prevention in our lifetime
- a. Look at the problem and change the individual
- b. Use education and equipment to protect the individual
- c. Change the environment both physically and culturally
Clinical Assistant Professor of Pediatrics and Family Medicine, The Ohio State University, Nationwide Children’s Hospital, Division of Sports Medicine, Web Editor, Clinical Journal of Sports Medicine
Brian Hainline, MD, CMO of the NCAA: Finding Solutions for the Youth Sports Injury Epidemic
• Sport specialization in early puberty develops the player, not the athlete.
• Our kids are arriving broken even before the arrive through our doors at the NCAA level
• Mental health issues are the #1 concern amongst our NCAA athletes
Rosemarie Moser, Ph.D., ABN, ABPP-RP: Cognitive Rest: Is It Really Best?
• Explains the important role of Neuropsychology in the Post-Concussive Athlete
• Addresses the “workaholic” culture and challenges the audience and parents “Do we really know how to rest?” and “are we modeling this for our youth?”
• Rest=best for concussion and delineates four key components of how to progress the student-adolescent athlete in a structured and overseen environment
Director, Sports Concussion Center of New Jersey, author of “Ahead of the Game: The Parents’ Guide To Youth Sports Concussion.”
Tracey Covassin, PhD, ATC: Gender Influences on Sport-Related Concussion Risks and Outcomes
• Females in sex comparable sports have higher rates of concussion than their male counterparts (basketball, ice hockey, lacrosse, and softball)
• Concussed females are cognitively impaired 1.7x more than male athletes
• You’ve evaluated an athlete on the field, now what? We must do due diligence and re-evaluate 24 and 48 hours post-injury
Associate Professor, Undergraduate Athletic Training Program Director, Michigan State University
Douglas J. Casa, PhD, ATC, FACSM, FNATA: Preventing Sudden Death in Youth Sports: The Challenges To Enacting Pro-Active Policies
• We need one singular goal: the development and implementation of policy in youth sports. Apropos policy changes can save lives
• 90% of all deaths in sport are from four causes (cardiac events, TBI, and heat illness)
• SMAC’s (sports medicine advisory committees) need to be comprised of sports medicine professionals like ATCs and MDs- not just policy makers who sit in a boardroom
Professor, Department of Kinesiology, Director, Athletic Training Education, Chief Operating Officer, Korey Stringer Institute, Research Associate, Human Performance Laboratory at the University of Connecticut
Allison Maurer, MS, RD, CSSD, CSCS: “What Do You Mean, You Didn’t Eat?”: The ABC’s of A High Performance Diet
• Nutrition is the missing link for our student athletes
• Our children are grossly overfed and severely undernourished
• Food=FUEL.
• We need to discuss fueling our athletes at 3 different levels: the athlete, the coach, and the parents
Sports Dietitian, University of Tennessee
Toben Nelson, ScD: Orange Slices and Hot Dogs: How the food environment in youth sports undermines its health benefits and what to do about it
• There is no difference in weight in our children who play a sport and who don’t. Our children are in an energy surplus
• Adults need to shape healthy food environments for our kids
• Provide youth sport volunteers with education to inspire real change
Associate Professor, School of Public Health, Division of Epidemiology & Community Health, University of Minnesota
Holly Silvers, MPT, PhD(Candidate): Injury Prevention in Youth Sports: Can We Increase Coaching Compliance and Design Cost-Effective Prevention Programs?
• Commented on the tremendous socioeconomic benefits for communities who implement ACL prevention programs
• $100/athlete savings w/respect to ACL prevention & screening programs see www.ncbi.nlm.nih.gov/pubmed/?term=24806006 for article
• Updated the audience on the differences of the FIFA 11+ v. the old FIFA 11
• Discussed the importance of neural preparedness before going into practice/competition
Director of Research, Santa Monica Sports Medicine Foundation, FIFA Medical Center of Excellence
Neeru Jayanthi, MD: Keeping Up With the Joneses: How Much Is Too Much in Youth Sports?
• We have to pay attention to the data at some point. Hours of training per week shouldn’t exceed a child’s age
• The more specialized you are in sport the more predisposed you are to injury
• It’s a perceived success with early sport specialization
Associate Professor, Department of Family Medicine, Orthopaedic Surgery and Rehabilitation, Medical Director, Primary Care Sports Medicine, Loyola University Chicago, Stritch School of Medicine
Rosalind Wiseman, Author and Mother: Navigating Youth Sports’ Troubled Waters: Concrete Strategies For Parents and Coaches
• Discussed the power of coaches and entrusting them with the emotional welfare of her children
• A call of action to create and sustain this social contract with our coaches and kids
• Adults don’t have the market cornered on emotional maturity. We have to manage ourselves so we can role model for our kids.
• Stand up for whats right when we hear youth using derogatory language and phrases like “that’s so gay” or “don’t be retarded”. Make these moments shocking and memorable
Best-selling author of Queen Bees and Wannabes and Masterminds and Wingmen: Helping Our Boys Cope With School Yard Power, Locker Room Tests, Girlfriends, and the New Realities of Guy World
Joe Ehrmann, Retired NFL Player & Motivational Speaker: InSideOut Coaching: How Sports Can Transform Lives
• We need transformational coaches to teach our youth to win with humility and lose with honor
• Coaches are educators. If we have student-athletes than we need teacher-coaches. We can’t just put a whistle in a math teachers possession and expect greatness.
• Discussing old school belittling coaching practices: Is it best practice or are we just repeating what was taught and how it was delivered
Katherine Starr: Best practices in Preventing Sexual Abuse in Youth Sports
• Addressed the uncomfortable conversation of sexual abuse in youth sports from a reflective, personal and informative role of advocate
Two-time Olympic Swimmer, Founder and Executive Director, Safe4Athletes
Donald Collins, JD: The View From the Commissioner’s Box: How Sports Officials Can Help Develop Athletes and Keep Them Safe
• Comprehensively and inspirationally reviewed officiating rules and roles in sport
Commissioner of Athletics, California Interscholastic Federation, San Francisco Section
Douglas E. Abrams, JD: The Power of the Permit in Youth Sports Safety
• Reviewed jurisdiction, paperwork, and permit laws pertinent to Youth Sports Safety
Professor of Law, University of Missouri School of Law
Deron Colby, JD: To an Athlete Dying Young: Why the Time for SmartTeams™ Is Now
• Poignantly connects with the audience discussing the array of medical errors and red flags missed over his 17 year old nephew, Matthew Colby’s, fatal concussion history
Janus Capital Law Group, PC and Co-Founder Matthew Colby Foundation