Nutrition 101 Series for Healthcare Providers:
Keeping Healthy Eating Simple for You and Your Patients Part II
Metabolism of Sugar: How Added Sugars Lead to Weight Gain
By Jenna Larsen, MS
“Food was just as abundant before obesity’s ascendance. The problem is the increase in sugar consumption. Sugar both drives fat storage and makes the brain think it is hungry, setting up a vicious cycle”- Robert Lustig, MD, University of California San Francisco [1]
A calorie is a calorie is a calorie.
This is a notion that America has been taught to believe, allowing consumers the freedom to trust that any food from the supermarket or restaurant has a place in our diet- as long as we manage to balance calories in with calories out.
And yes- it’s true. If we can balance calories, weight will not increase. So why has it become so difficult to maintain a healthy weight? Consider that 1) a significant increase in added sugars has seeped into the U.S. food supply since the 1970s; and 2) the way that sugar affects our brain and eating behaviors is unlike any other food particle we consume.
The onset of the obesity epidemic directly correlates with the advent of the U.S. dietary guidelines in 1977 [2]. As a result of the recommendation to decrease fat consumption, food companies dialed down the fat in their products while substituting sugar to maintain palatability [3]. The result…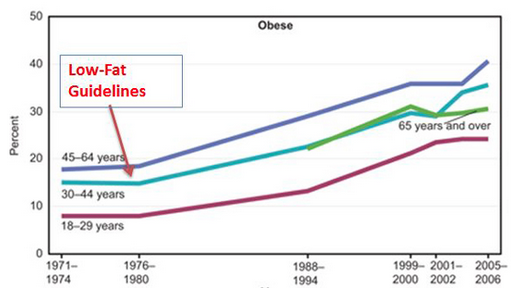
Americans doubled their intake of sugar by 2000 and 80% of products available in the supermarket now contain added sugar [4]. What we lacked was an understanding of how sugar hijacks the brain’s ability to recognize satiety leading to an overall increase in total calorie consumption.
Comprehending how added sugars are processed for energy helps explain why calories from different foods have varying impacts on fat storage and appetite. Consider 150 calories from an apple versus 150 calories from apple juice.
When you eat an apple, the fiber allows the sugar to gradually absorb into the bloodstream. Insulin is steadily released and glucose is taken into cells where it is used for energy. However, unlike an apple, apple juice lacks fiber. So instead of a gradual release, the bloodstream is bombarded with sugar. Insulin rises quickly, telling the liver to convert the sugar into fat for storage [5,6]. That newly formed fat is released into the bloodstream, blocking the effect of the satiety hormone, leptin [7]. The result? The brain tells you to eat more.
Furthermore, insulin spikes lead to blood sugar crashes, advancing the signal to the brain that you need to more food. These processes combine to induce lethargy and hunger that contributes to more eating, less physical activity, more fat formation, and overall weight gain [4].
In short- the calories in the apple lead to satiety and energy while the calories from the apple juice lead to hunger and lethargy- all due to the way sugar is metabolized.
The American Heart Association recommends just 6 grams of added sugar per day for women and 9 grams for men [8]. The average American consumes 80 grams of sugar per day [9] while a 12 ounce can of regular soda contains 32 grams of sugar [10]. Offering perspective as to how much added sugar we consume can help patients gain awareness and motivate them to make a change.
Supplement your discussion with these points:
- For an effective visual, fill empty bottles of soda, juice and a sports drink with the number of teaspoons of sugar they contain (1 gram= 4 teaspoons). Patients will be surprised at how much sugar they are drinking when they see it presented in this way.
- All sugars are processed the same way. White bread, white rice, and potatoes are no different than other types of sugar. Purchasing whole grain products keep the fiber intact so that the sugar is absorbed more gradually.
- Food consumed closest to its natural form will have fewer added sugars and more fiber. Preparing fruits and vegetables is the best way to ensure that metabolism is functioning properly (Nutrition 101: Whole Foods)
- Added sugars go by many different names, yet they are all a source of extra calories. Click here for a list of added sugars that doubles as a handout for patients.
- Just as our palates have been conditioned to crave sugar, they can be conditioned to crave it less [4]. Coffee drinkers can train their palate by gradually decreasing the number of sugars while soda drinkers can start by diluting them with water.
The link between sugar consumption and chronic disease is not a new concept. In fact, more than 8,000 scientific papers have been published on the health effects of added sugars [11]. By investing a few minutes to discuss their importance, you play a key role in drastically improving patients’ overall health and well-being.
References:
- https://www.ucsf.edu/news/2009/06/8187/obesity-and-metabolic-syndrome-driven-fructose-sugar-diet
- Source: National Center for Health Statistics (US). Health, United States, 2008: With Special Feature on the Health of Young Adults. Hyattsville (MD): National Center for Health Statistics (US); 2009 Mar. Chartbook.
- http://www.npr.org/blogs/thesalt/2014/03/28/295332576/why-we-got-fatter-during-the-fat-free-food-boom
- Fed Up Movie
- Newman, Cathy. “Why are we so fat.” National Geographic 206.2 (2004): 46-62.
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC380258/
- http://diabetes.diabetesjournals.org/content/53/5/1253.full.pdf
- http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyEating/Added-Sugars_UCM_305858_Article.jsp
- http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyEating/Added-Sugars_UCM_305858_Article.jsp
- http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyDietGoals/Frequently-Asked-Questions-About-Sugar_UCM_306725_Article.jsp
- https://www.ucsf.edu/news/2014/11/120751/ucsf-launches-sugar-science-initiative